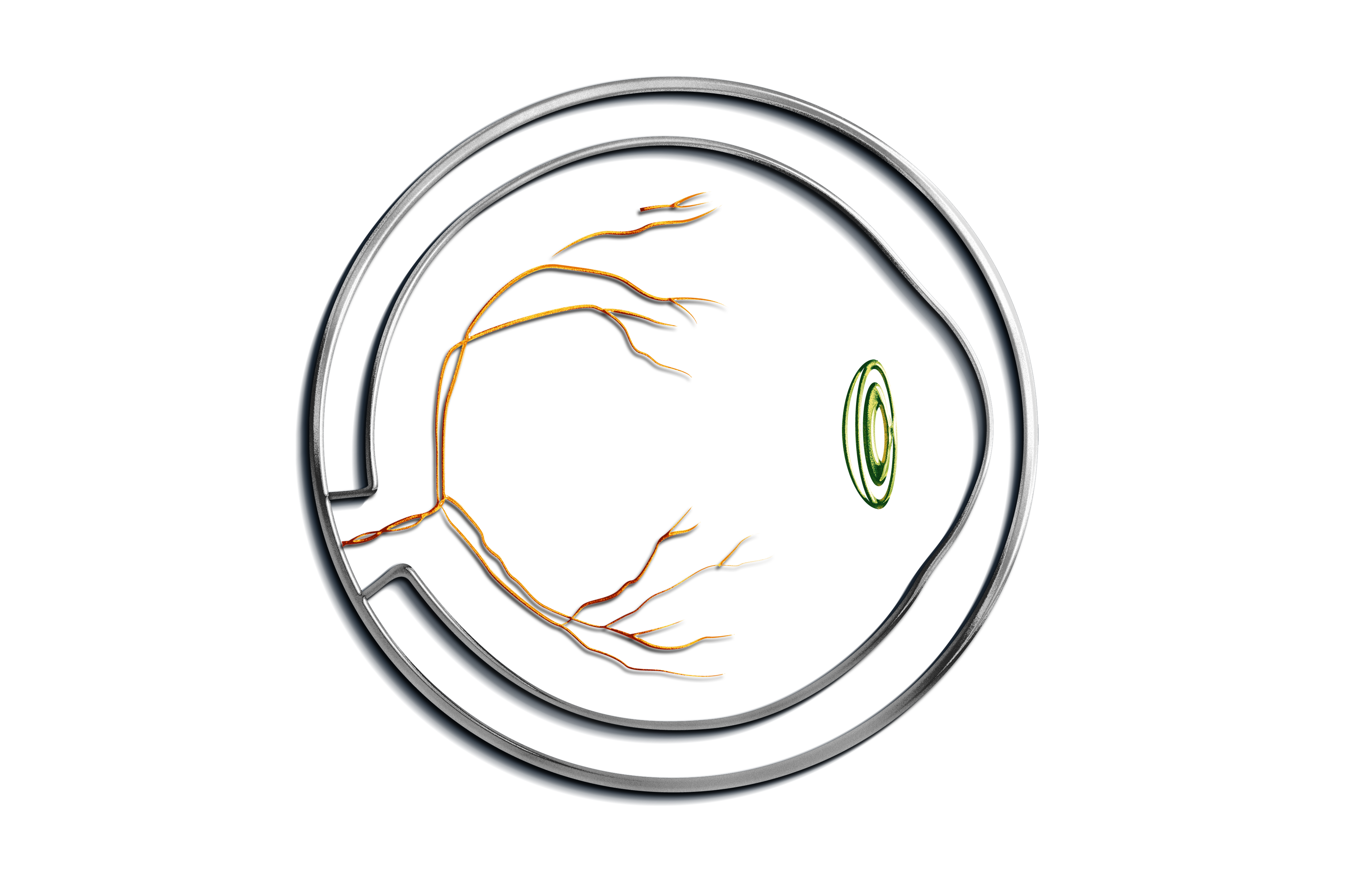
SAFETY AND FEASIBILITY OF A NOVEL 25-GAUGE BIODEGRADABLE IMPLANT OF DEXAMETHASONE FOR TREATMENT OF MACULAR EDEMA ASSOCIATED WITH RETINAL VEIN OCCLUSION: A PHASE I CLINICAL TRIAL Renato B. Cunha, MD,* Rubens C. Siqueira, MD, PhD,* André Messias, MD, PhD,* Ingrid U. Scott, MD, MPH,† Silvia Ligorio Fialho, PhD,‡ Armando da Silva Cunha- Junior, PhD,§ Rodrigo Jorge, MD, PhD* Purpose: To evaluate the safety and feasibility of a 25-gauge biodegradable implant containing 350 mg of dexamethasone (DDS-25) for the treatment of decreased vision due to macular edema associated with central or branch retinal vein occlusion. Methods: Prospective, nonrandomized, open-label, Phase I clinical trial, including 10 patients with decreased vision (best-corrected early treatment diabetic retinopathy study visual acuity of 20/40 or worse) due to macular edema associated with central retinal vein occlusion (n = 4) or branch retinal vein occlusion (n = 6) for more than 4 months. Comprehensive ophthalmic evaluation, including best-corrected visual acuity, spectral domain optical coherence tomography (Spectralis Heidelberg Engineering) for determina- tion of central subfield thickness, full-field electroretinography (ISCEV standard ERG), and fluorescein angiography, was performed at baseline, and 1, 4, 12, and 24 weeks after intravitreal DDS-25 insertion. Results: Mean best-corrected visual acuity was 0.72 ± 0.1 logMAR (20/100) at baseline and improved by 7 early treatment diabetic retinopathy study letters to 0.58 ± 0.08 logMAR (20/80 + 1) at 24 weeks (P = 0.049), with 3 central retinal vein occlusion and 3 branch retinal vein occlusion patients improving between 1 and 4 early treatment diabetic retinopathy study lines. Significant central subfield thickness reduction was observed at 24 weeks compared with baseline (P = 0.011); mean ± standard error (range) central subfield thickness (mm) was 461.2 ± 41.3 (288–701) at baseline, and 439.6 ± 40.4 (259–631), 442.5 ± 44.6 (255–632), 354.6 ± 31.2 (228–537), and 316.5 ± 26.4 (226–441) at 1, 4, 12, and 24 weeks, respectively. No significant changes in electroretinography responses or area of retinal nonperfusion were observed during 24 weeks of follow-up. There was no significant change in mean intraocular pressure at any of the study visits compared with baseline. One patient had mild anterior chamber inflammation (1–5 cells) at one week after DDS-25 insertion. Conclusion: In this Phase I study demonstrating the feasibility of intravitreal DDS-25 insertion for the treatment of decreased vision due to macular edema associated with retinal vein occlusion, no safety concerns were observed. A larger prospective randomized study with longer follow-up is warranted to confirm these findings. RETINAL CASES & BRIEF REPORTS 0:1–9, 2016